Rural Primary Health Care Memory Clinics Provide Assessment and Post-diagnostic Support Close to Home
CCNA Knowledge Mobilization Activity (2024)
“It is so important to older adults to have local health care and not have to travel many miles.”


- Members of the Rural Dementia Action Research (RaDAR) Team at the University of Saskatchewan are facing the challenge of improving the delivery of rural dementia care, including specialist care, primary healthcare, remote service delivery, and use of technology.
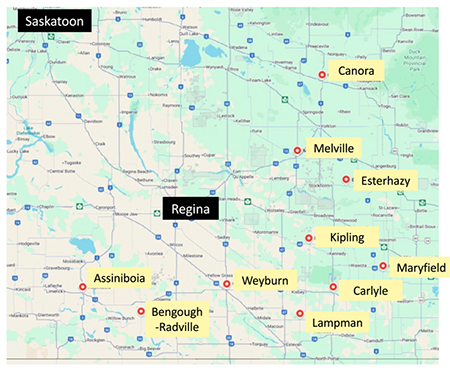
- Local one-day team-based memory clinics are intended to reduce travel and wait times for specialist appointments, providing coordinated care and supports for patients and families in their home community. These clinics, delivered by local healthcare professionals, have been implemented and sustained in ten (10) communities in Saskatchewan to date, with additional clinics in planning stages.
- The memory clinics core elements are:
- Interprofessional Care: family physician/nurse practitioner, home care nurse, social worker, physical therapist, occupational therapist, pharmacist, dietitian, and Alzheimer Society First Link Coordinator (team composition varies by community);
- Decision Support: electronic medical record-based assessment flow sheets with sections for each team member; and,
- Specialist-to-Provider Support: training, continuing education, access to RaDAR Specialist Memory Clinic.
-
The realized impact of these clinics is that patients and families valued the comfort and convenience of local care, “being heard”, being in the same room and “same page” with the entire team and receiving help for the future. The majority felt free to talk about their concerns, learned about available supports and what to expect, and felt the team approach was helpful. Family members shared:
“It is wonderful to see this clinic in a small town. It is so important to the elderly to have local health care and not have to travel many miles.”
“This was the first time we had any discussion about what was going to happen…Finding some answers, knowing there is help… it was like phew, ok, I don’t have to do this myself.”
- One month after initial assessment, care partner self-efficacy had increased, and fewer care partners reported unmet service/support needs. Team members felt more confident, and report assessments are more comprehensive and coordinated.
- Next steps include:
- Continuing to expand the clinics geographically while supporting the sustainability of existing clinics;
- Continued research on clinic outcomes; and,
- Evaluating hybrid in-person/virtual models.
About the Team
- Dr. Megan E. O’Connell, Professor, Dept of Psychology & Health Studies, University of Saskatchewan.
- Dr. Debra Morgan, Professor, Canadian Cente for Rural & Agricultural Health, University of Saskatchewan.
- Dr. Julie Kosteniuk, Assistant Professor, Canadian Centre for Rural & Agricultural Health, University of Saskatchewan.
Drs. O’Connell and Morgan are co-leads of the Canadian Consortium on Neurodegeneration in Aging (CCNA) Team 15 (Issues in Dementia Care for Rural Populations) and investigators on the RaDAR team, funded by CCNA.
Team 15 research focuses on development/spread/sustainability of rural primary care memory clinics, health service use (Drs. Morgan, Kosteniuk), remote service delivery, use of technology for remote specialist care (Dr. O’Connell), and collaborates with Team 18 on Issues in Dementia Care for Indigenous Populations (led by Drs. Crowshoe and Walker) including with the Canadian Indigenous Cognitive Assessment (CICA).
Links to key/related outputs, including academic and non-academic, and further reading:
- A 5-step approach for developing and implementing a rural primary health care model for dementia: A community-academic partnership (Primary Health Care Research & Development)
- Barriers and Facilitators to Development and Implementation of a Rural Primary Health Care Intervention for Dementia: A Process Evaluation (BMC Health Services Research)
- Factors influencing sustainability and scale-up of rural primary healthcare memory clinics: perspectives of clinic team members (BMC Health Services Research)
- Perceptions and outcomes of an embedded Alzheimer Society First Link Coordinator in rural primary health care memory clinics (BMC Health Services Research)
- Services for older adults in rural primary care memory clinic communities and surrounding areas: a qualitative descriptive study (BMC Health Services Research)
- Collaborative approaches to team-based primary health care for individuals with dementia in rural and remote settings: A scoping review (Canadian Journal on Aging)
- Date modified: